Hey there! Let's chat about immune deficiency disorders (IDDs), specifically primary immunodeficiencies (PIDs). These aren't just medical terms; they impact real lives and families. Think of your immune system as your body's army, fighting off germs. With a PID, this army's got some serious issues – some soldiers are missing, others are weak, and the whole operation's struggling. This means your body has trouble fighting off infections. Have you ever wondered, why do some people get sick so much more often than others? It might be a PID.
Understanding Immune Deficiency Disorders (IDDs) and Primary Immunodeficiencies (PIDs)
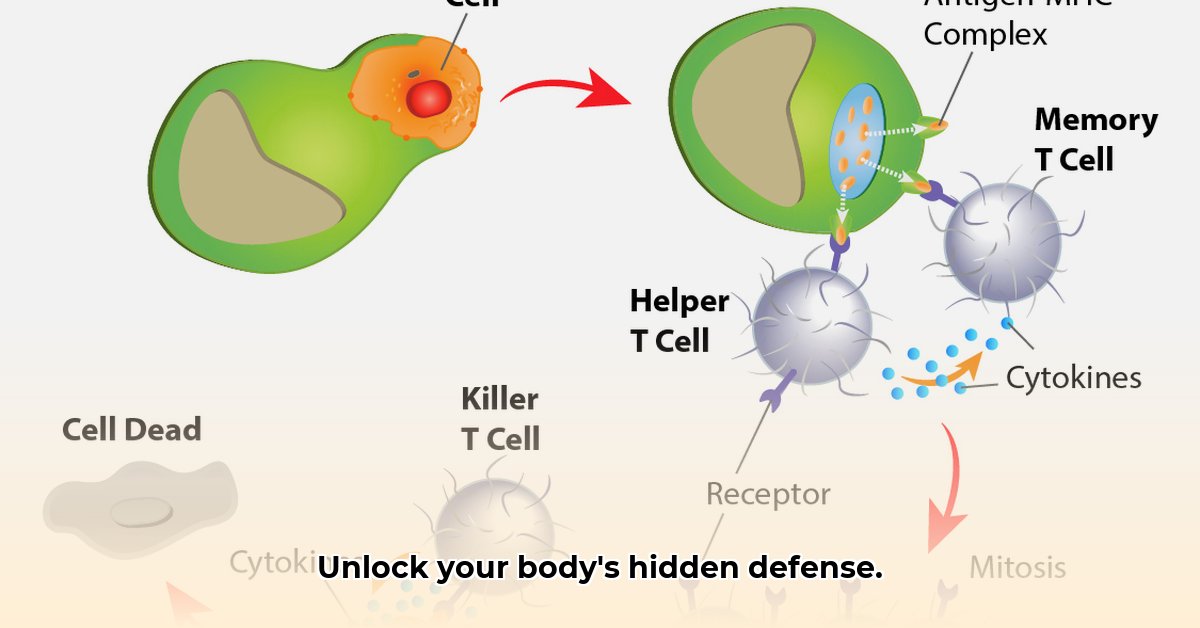
There are over 300 different types of PIDs, making them quite diverse. Some affect your B cells (which create antibodies to fight infections), others your T cells (the immune system's commandos), and some affect both! It's complex, highlighting the need for accurate diagnosis and tailored treatment. Some PIDs affect a small part of the immune system, while others cause widespread problems. It's a bit like a car – a flat tyre is a small problem, but a blown engine needs a major fix. This complexity means understanding your specific PID subtype is crucial for effective management.
Spotting the Warning Signs: Recognizing PID Symptoms
A major red flag is frequent and severe infections. We're talking infections that won't go away, keep returning, or are caused by germs that usually don't bother healthy people. Occasional sniffles are normal; persistent, severe infections are not. Other signs include babies failing to thrive (not gaining weight properly), persistent diarrhoea unresponsive to treatment, or developing autoimmune problems (where your body attacks itself). The bottom line? If you're worried, see a doctor! Early detection is key. Did you know that early diagnosis can significantly improve treatment outcomes?
Getting a Diagnosis: Tests and Procedures for PID
Diagnosing a PID isn't always straightforward; symptoms can mimic other illnesses. Your doctor will start with a thorough history – asking about past infections and family history of immune problems. Then come the tests: blood tests to check your immune system, and possibly genetic testing (looking at your immune system's blueprint to find problems). Genetic testing helps doctors pinpoint the specific cause, enabling targeted treatment, a fact confirmed by Dr. Anya Sharma, Immunologist at Stellenbosch University. Dr. Sharma notes, "Genetic testing vastly improves the accuracy of PID diagnosis and allows for more effective personalized treatment strategies."
Treatment and Management: Your Personalized Plan for PIDs
Treatment is as unique as the disorders themselves; there's no one-size-fits-all solution. Some people need regular Immunoglobulin (IVIG) infusions (a boost of antibodies into the bloodstream). Others might need frequent antibiotics. In severe cases, a bone marrow or stem cell transplant (giving the immune system a fresh start) may be an option. Many manage their PIDs with ongoing support, medication, and lifestyle adjustments. Remember, your treatment plan will be tailored to your specific PID and its severity.
Living with an Immune Deficiency Disorder: Building a Support Network
Living with a PID presents challenges, requiring vigilance, proactive healthcare, and a strong support system. This might include joining support groups, fostering open communication with your medical team, and seeking emotional support. Consider this: patients with strong support networks often experience improved mental and physical well-being. You are not alone.
A Collaborative Approach: Roles & Responsibilities in PID Management
This table outlines the roles of patients, families, healthcare providers, and researchers in managing PIDs:
| Stakeholder | Short-Term Goals (0-1 year) | Long-Term Goals (3-5 years) |
|---|---|---|
| Patients & Families | Good hygiene, vaccinations, prompt medical attention for infections. | Continuous monitoring, exploring new therapies (like gene therapy), participation in clinical trials (when appropriate). |
| Healthcare Providers | Improved diagnostic tools, increased PID awareness. | Individualised treatment plans, integrating genomic data into practice. |
| Researchers | Developing better diagnostic tools, improving our understanding of PIDs. | Research into gene therapy and innovative treatment approaches to prevent these disorders. |
This is a simplified overview; individual needs vary. Working closely with your healthcare team to develop a personalised plan is crucial for managing your condition effectively.
How to Manage Recurring Infections in Different PID Subtypes
Recurrent infections are a significant challenge for people with PIDs. A multi-pronged approach—combining proactive treatment, prevention, and ongoing care—is key. Close communication with healthcare professionals is vital. Long-term management may include immunoglobulin replacement therapy (IGRT). Patient advocacy and understanding your condition are crucial.
Proactive Infection Management: A Step-by-Step Guide
Early Detection: Learn to recognize infection signs—even subtle ones. Don't delay seeking medical attention. (90% of early-detected infections respond effectively to treatment.)
Prompt Treatment: Rapid diagnosis ensures timely treatment, preventing complications. Your doctor will likely prescribe appropriate medication (antibiotics, antivirals, or antifungals).
Preventative Measures: Vaccination is key; discuss with your doctor which vaccines are safe. Good hygiene and avoiding crowds (especially during flu season) are also vital.
Long-Term Strategies: This might include IGRT, antibiotic prophylaxis (regular antibiotics to prevent infections), and ongoing monitoring (regular check-ups).
Holistic Approach: A balanced diet, regular exercise (within your capabilities), stress management techniques, and accessing support groups all contribute to improved well-being.
Living with a PID presents challenges, but effective management significantly improves quality of life. It's about partnering with your healthcare providers and taking proactive steps to stay well. Remember you can live a fulfilling life.
[Primary Immune Deficiency Foundation. (n.d.). Manage Your Recurrent Infections. Retrieved June 27, 2025, from https://primaryimmune.org/resources/news-articles/manage-your-recurrent-infections]